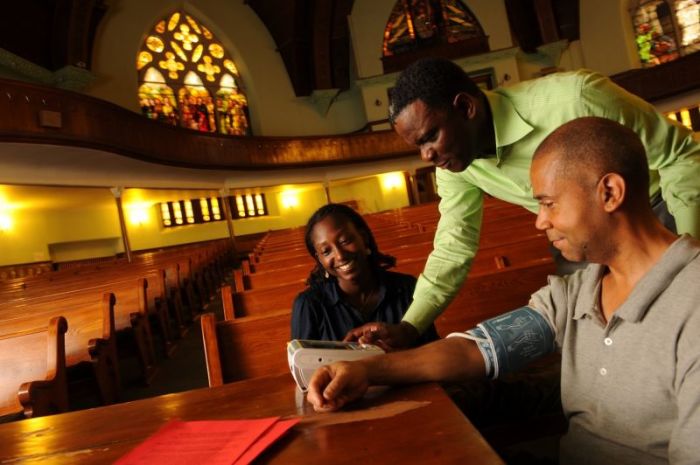
Study Shows Churches Can Help Reduce High Blood Pressure in Black Communities
African-Americans who get comprehensive lifestyle advice in a motivational church environment from community-based health workers experience significant reductions in high blood pressure compared those who just get health education alone, according to a new study conducted by researchers at the NYU School of Medicine.
The study, published in the journal Circulation: Cardiovascular Quality and Outcomes, is the first and largest community-based study that evaluates the effect of comprehensive lifestyle intervention on reducing blood pressure among African-Americans in black churches.
"African-Americans have a significantly greater burden of high blood pressure and heart disease, and our findings prove that people with uncontrolled high blood pressure can, indeed, better manage their blood pressure through programs administered in places of worship," Dr. Gbenga Ogedegbe, a professor of Population Health and Medicine at NYU School of Medicine and the study's lead author, said in a release. "Vulnerable populations often have lower access to primary care. We need to reduce racial disparities in hypertension-related outcomes between blacks and whites. Additionally, we hope clergy and church leaders will take note of our findings and replicate these interventions in their churches."
In 2013, NYU Langone Medical Center announced that Ogedegbe received a $12 million five-year grant from The National Institute of Neurological Disorders and Stroke of the National Institutes of Health, to create a new Center for Stroke Disparities Solutions in New York City.
It was part of a broader $40 million effort to examine racial, ethnic, and socioeconomic risk factors of stroke and to eliminate disparities in stroke incidences in the U.S. Blacks and Hispanics continue to experience worse stroke-related outcomes than whites.
The results of this latest study offers a solution toward ending some of those disparities.
Data was collected for the study from 2010 to 2014 and involved 373 participants from New York City churches who identified as black and self-reported a diagnosis of high blood pressure and uncontrolled blood pressure.
The participants were then divided into two groups. One, called the MINT-TLC group, attended 11 90-minute weekly group sessions focused on making healthy lifestyle changes, according CNN. The sessions were run by members of the church who served as lay health advisers. The sessions were then followed up with three monthly progress phone calls to a group leader.
The second group of participants got one lifestyle session focused on high blood pressure. They also received 10 sessions from health experts on another topic such as Alzheimer's disease or fire safety but they did not get motivational calls.
The group that got motivational calls showed clinically significant improvement in their blood pressure.
"The lay health model was a good one to have as part of the design," Mimi Kiser, a research assistant professor at Emory University's Rollins School of Public Health, who was not involved in the study, told CNN. "It fits well into the culture of the church and also into effective community-based strategies."
Dr. Joseph Ravenell, associate professor of population health and medicine at the New York University School of Medicine, said the study "supports the notion that non-clinicians based in the community can be effective messengers for healthful behavior change in blacks with high blood pressure."




























